The use and overuse of antibiotics in food, medications and industry is among the most concerning trends in healthcare over the last 50 years. The World Health Organization (WHO) and the Center for Disease Control (CDC) each have statements describing the importance of preventing the overuse and over-prescribing of antibiotics.
It’s not uncommon to get a secondary infection when your immune system is already compromised. The beauty of text-based care through 98point6 is that if you aren’t feeling better—or if you start feeling worse—you can start a follow-up visit as soon as you need to, 24/7, from wherever you are. No waiting for another appointment or skipping work to go back to urgent care. At that time, we’re happy to address whatever new or lingering symptoms you may be experiencing and continue guiding you in the right direction.
With so much information out there, it’s hard to know what you should be doing and how worried you should be. Here are some key things to keep in mind, according to the Centers for Disease Control and Prevention (CDC).
1. Most common symptoms of COVID-19 include fever, dry cough and tiredness. Some patients may have aches and pains, nasal congestion, runny nose, sore throat or diarrhea.
2. So far, children seem to be having milder cases than adults. Older individuals, and those with underlying medical problems like high blood pressure, heart problems, lung conditions or diabetes are more likely to develop serious illness, as well as people with a history of smoking.
3. Physical distancing is crucial in stopping the spread.The CDC is encouraging Americans to maintain a physical distance of approximately 6 feet, when possible, in indoor and outdoor public spaces. Since people can pass the virus to others before they know they are sick—and if they aren’t even experiencing symptoms—this measure reduces the opportunity for disease transmission, protecting high-risk communities and helping to stop the spread as a whole.

4. Wearing a mask in public settings may also help stop the spread. The CDC has updated its guidance on wearing cloth face coverings, including bandanas and scarves. This is less to protect you and more to prevent the spread of COVID-19 to others, since many people who are infected experience mild to no symptoms. Unless you already have one, surgical masks and N-95 respirators should not be purchased, since they are in short supply and critically needed for healthcare workers. You can learn how to easily make your own cloth face covering using a T-shirt and scissors from the CDC.
5. Trust the right resources. Media can be a powerful tool, but what you’re hearing may not be accurate. For the most up-to-date information, frequently check back with the CDC or World Health Organization (WHO) websites.
Asthma is a common and lifelong chronic disease characterized by an inflamed airway that leads to decreased air flow. As a result, asthmatics experience uncomfortable and scary symptoms including wheezing, coughing and shortness of breath.
While it tends to run in families, asthma can also be related to factors such as allergies, age and environment. Triggers include allergens such as dust or pets and other medical conditions, like the common cold.
There’s a misconception that asthma starts only in children. With an idiopathic asthma diagnosis, an adult who has never had the condition can develop it later in life. (Similarly, adults who have controlled their symptoms since childhood can start struggling with asthma control once again as they age.) Obesity, hormonal fluctuations and prolonged exposure to certain irritants may all be linked to the development of adult-onset asthma.
Use this handy checklist to determine if you or someone in your family might have symptoms commonly associated with asthma.
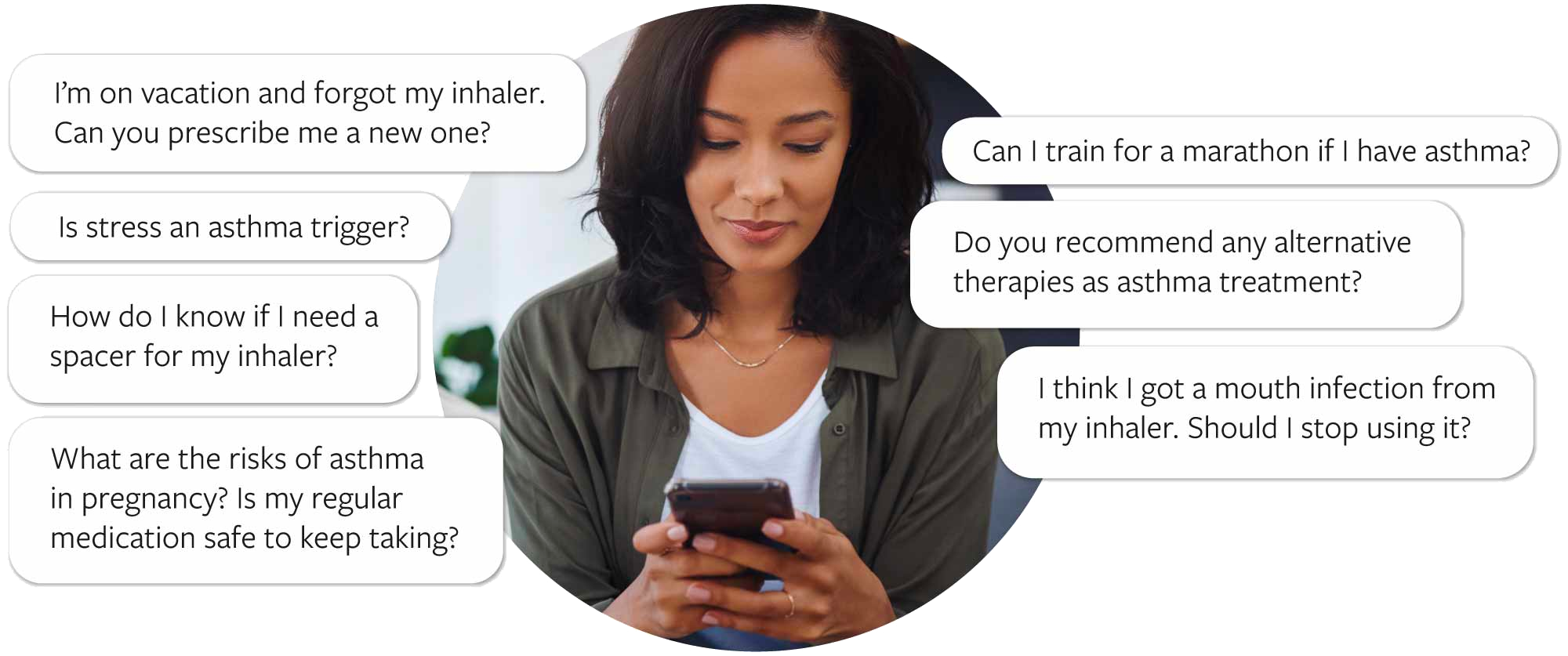
Need help keeping your asthma under control? Here are some questions and concerns that can be easily addressed, 24/7, by a 98point6 physician.
Losing weight, eating healthier and exercising more are the most consistently popular New Year’s resolutions—especially after so much overindulging during the holidays. Chances are you’ll be hearing a lot of buzz about the latest miracle diet or healthy eating program. You may even be tempted to try one.
The truth is that food is medicine. And like the prescription your physician calls into the pharmacy, what’s on your plate should be suited to your age, individual needs and personal lifestyle. This is why checking in with an actual doctor is always highly recommended before embarking on any significant change to your diet.
“Although there are a lot of dieting trends, one of the most consistent factors in healthy eating is limiting ultra-processed food in favor of higher-quality foods such as whole grains, fresh fruits and vegetables, and homemade snacks and salad dressings.”
-Erin Jones, MD
Working closely with a physician is especially crucial if the individual who is unhappy with their weight is a child or teen. Kids going through puberty or preparing for a growth spurt need to eat more than an adult who isn’t going through such a rapid state of change, so adhering to a 2,000-calorie per day diet is rarely appropriate for them. Plus, everyone’s bodies are unique: even identical twins can respond differently to the exact same foods!
No matter what your age, if the goal is weight loss, it’s always important to keep a healthy outlook. That includes paying attention not only to how much you’re eating, but also to how often you’re thinking about diet and food control. Based on my professional experience in relation to eating disorders—which includes treating them in both inpatient and outpatient contexts, teaching nurses, medical students and healthcare providers and collecting clinical data regarding eating disorders and refeeding syndrome—I would flag the following warning signs as a possible cause for concern.
If you recognize any of the behaviors above in yourself or someone you care about, reach out to a physician for trusted guidance and support.
Whether your child has a fever or you’re worried about that dizziness you’ve been feeling, 98point6 is available 24/7 to you and your eligible family members ages 1 and older. With access to on-demand primary care via a mobile app, care is always at your fingertips.